Understanding Sperm Morphology: A Guide to Male Fertility
Estimated Reading Time: 8 minutes
Table of Contents
Male fertility is a complex subject with many contributing factors, and understanding semen morphology is a crucial piece of the puzzle. It refers to the size and shape of sperm, which is a key indicator of sperm health evaluated during a semen analysis. While it may sound like a highly technical term, its implications are significant for couples trying to conceive.
Abnormal morphology, also known as teratozoospermia, can impact a sperm’s ability to fertilize an egg. This comprehensive guide will explore the various aspects of morphology, from its causes and diagnostic methods to potential treatments and lifestyle changes that can positively influence sperm health, providing a clearer picture of this important aspect of reproductive medicine.
The Etiology of Abnormal Sperm Morphology
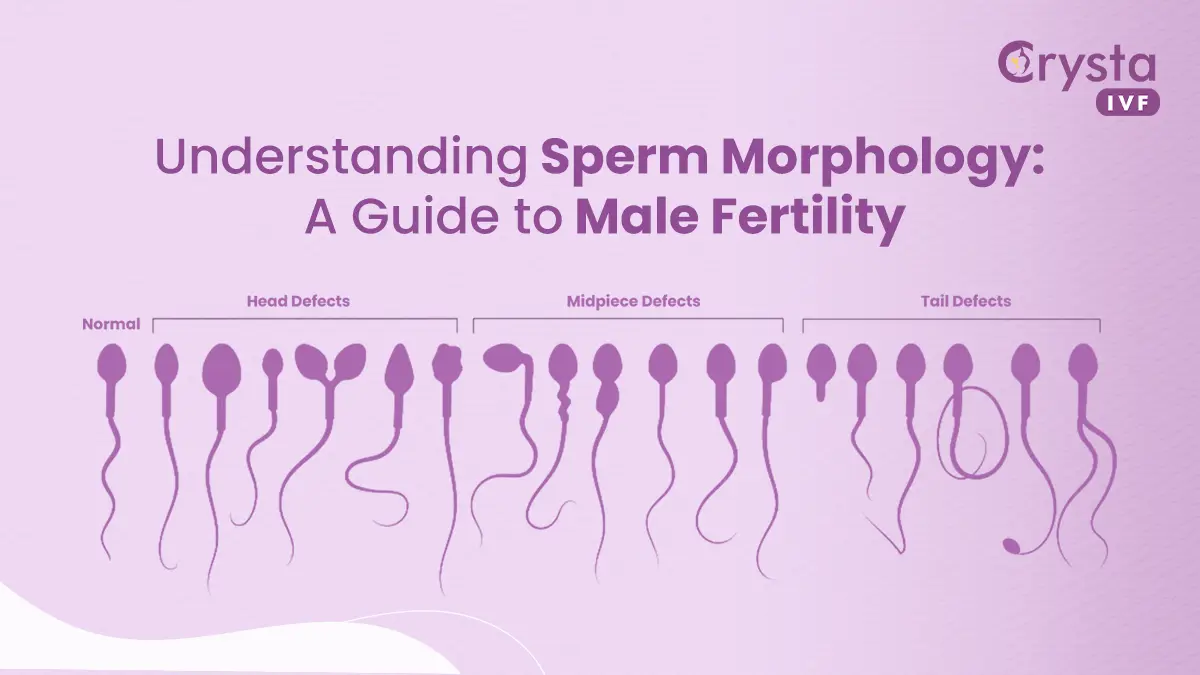
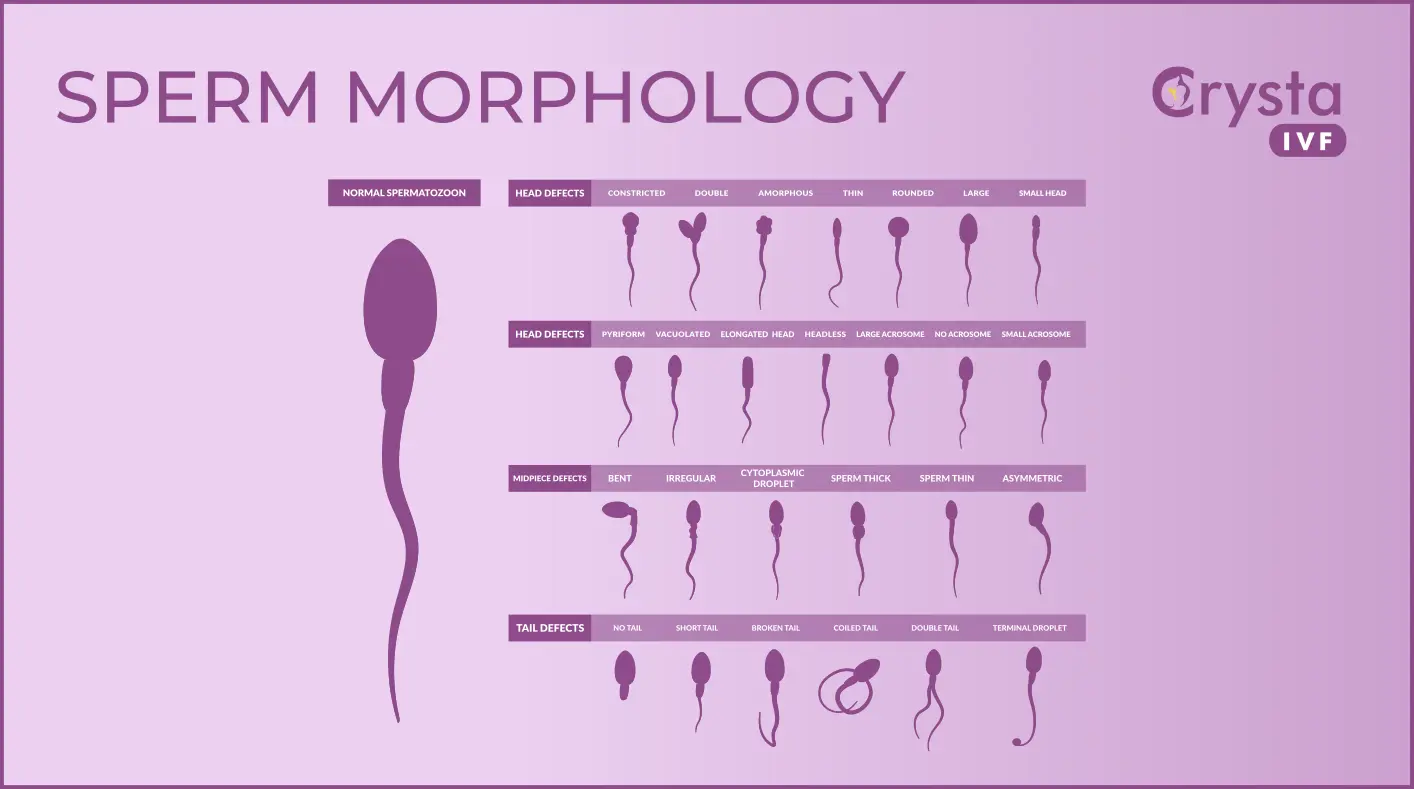
The causes of abnormal sperm morphology are varied and can range from genetic predispositions to environmental influences and lifestyle choices. Identifying the specific etiology is essential for determining the most effective course of action. Genetically, certain inherited conditions can directly affect spermatogenesis – the process of sperm production – leading to a higher percentage of malformed sperm. These defects can impact the sperm’s head, midpiece, or tail, hindering its motility and ability to penetrate an egg. Hormonal imbalances, such as low testosterone or issues with the pituitary gland, also play a significant role.
These hormones are critical for regulating sperm development, and any disruption can lead to abnormalities in their final form. A complete understanding of the etiology of abnormal morphology is the first step toward addressing potential fertility challenges and developing a targeted treatment plan.
Furthermore, lifestyle and environmental factors contribute heavily to issues with morphology. Exposure to certain toxins, such as pesticides, heavy metals, and industrial chemicals, has been shown to have a detrimental effect on sperm quality. Similarly, lifestyle habits like smoking, excessive alcohol consumption, and the use of illicit drugs can impair sperm production and structure. Oxidative stress, which is an imbalance between free radicals and antioxidants in the body, is another major contributor.
This cellular damage can affect sperm DNA integrity and morphology. Elevated scrotal temperature, caused by factors like tight-fitting underwear, frequent use of hot tubs, or prolonged sitting, can also disrupt the delicate environment needed for healthy sperm development. Addressing these modifiable risk factors is often a primary recommendation for improving overall sperm health.
“The art of medicine consists of amusing the patient while nature cures the disease.” – Voltaire
Signs and Symptoms of Poor Morphology
One of the most challenging aspects of abnormal morphology is that it typically presents with no outward signs or symptoms. A man can feel perfectly healthy and have a normal libido and sexual function, yet have a high percentage of abnormally shaped sperm. The primary—and often only—”symptom” is difficulty conceiving a child, or male factor infertility. Because the condition is asymptomatic, it often goes undiagnosed until a couple seeks medical advice after trying to get pregnant for an extended period without success. This lack of visible indicators underscores the importance of a comprehensive fertility evaluation for both partners when conception does not occur within a reasonable timeframe, which is generally considered one year for couples under 35 and six months for those over 35.
While there are no direct physical symptoms, the underlying causes of poor morphology might have their own set of signs. For instance, if a hormonal imbalance is the root cause, a man might experience symptoms like decreased sex drive, erectile dysfunction, loss of body hair, or fatigue. If a varicocele (an enlargement of the veins within the scrotum) is contributing to the issue, there might be a noticeable lump or swelling in the scrotum, or a dull, aching pain. However, these signs are not specific to abnormal morphology and can be indicative of various other medical conditions. Therefore, the definitive method for identifying issues with sperm shape and size remains a microscopic examination of a semen sample, making a professional medical diagnosis indispensable.
Diagnosing and Understanding Sperm Morphology
The diagnosis of abnormal sperms is made through a sperm morphology analysis, which is a cornerstone of male fertility testing. During this laboratory test, a sample of semen is examined under a high-powered microscope to assess several parameters, including sperm count, motility (movement), and morphology. For the morphology assessment, a technician stains the sperm cells to make them visible and evaluates the shape and size of hundreds of individual sperm. The results are reported as the percentage of normally shaped sperm. Different classification systems exist, with the Kruger’s strict criteria being one of the most commonly used. According to these strict guidelines, a sample is considered normal if 4% or more of the sperm have a perfect shape. This might seem like a very low number, but it reflects the high standards used for evaluation.
Interpreting the Results of a Sperm Morphology Test
Understanding the Sperm Morphology Results requires careful interpretation by a fertility specialist. A result showing less than 4% normal forms does not automatically mean that natural conception is impossible. It simply indicates that the chances may be lower because fewer sperm are well-equipped to travel through the female reproductive tract and fertilize an egg. It is also important to consider that semen parameters can fluctuate significantly over time. A single poor result may not be representative of a man’s overall fertility potential. Therefore, doctors often recommend repeating the semen analysis after a few months to confirm the findings, especially if lifestyle modifications have been implemented in the interim. A comprehensive diagnosis of sperms involves looking at the complete picture of male reproductive health.
The Role of Advanced Testing in Sperm Morphology
In some cases, a standard semen analysis may be followed by more advanced tests to gain deeper insights into sperm function and its impact on fertility. For example, a sperm DNA fragmentation test measures the amount of damage to the genetic material within the sperm. High levels of DNA fragmentation can be linked to poor embryo development and miscarriage, even if morphology report appears normal. These advanced diagnostic tools can help fertility specialists create a more personalized treatment strategy. By combining the findings from various tests, a doctor can better understand the specific challenges related to a patient’s semen morphology and recommend the most appropriate interventions, from lifestyle changes to assisted reproductive technologies like IVF or ICSI.
Data Table for comparing World Health Organization (WHO) and Kruger’s Strict Criteria for normal semen analysis parameters.
| Parameter | WHO 5th Edition (Lower Reference Limit) | Kruger’s Strict Criteria |
| Sperm Concentration | 15 million/mL | >20 million/mL |
| Total Motility | 40% | >50% |
| Progressive Motility | 32% | >25% |
| Normal Morphology | 4% | >4% (some labs use >14%) |
Treatments and Improvements for Sperm Morphology
While a diagnosis of poor semen morphology can be concerning, there are several pathways for treatment and improvement. The approach depends heavily on the underlying cause. For men whose abnormal sperm shape is linked to lifestyle factors, making positive changes can have a significant impact. This includes quitting smoking, reducing alcohol intake, and maintaining a healthy weight through a balanced diet and regular exercise. A diet rich in antioxidants, found in fruits, vegetables, and nuts, can help combat oxidative stress and protect developing sperm. Specific nutrients like zinc, selenium, Coenzyme Q10, and L-carnitine have also been linked to improved sperm health, and supplementation may be recommended by a doctor.
When lifestyle changes are not sufficient or the cause is medical, other treatments are available. If a varicocele is identified, a surgical procedure called a varicocelectomy can be performed to repair the enlarged veins, which often leads to improvements in sperm parameters, including morphology. Hormonal imbalances can be corrected with medication to restore normal sperm production. For many couples, assisted reproductive technology (ART) offers the most direct route to pregnancy. Intrauterine insemination (IUI) may be an option if morphology issues are mild. For more severe cases of teratozoospermia, in vitro fertilization (IVF) with intracytoplasmic sperm injection (ICSI) is highly effective. ICSI involves injecting a single, carefully selected sperm directly into an egg, bypassing many of the natural barriers that an abnormally shaped sperm would face.
Crysta IVF Patient Testimonial
“After a year of trying, we learned that my husband’s semen morphology was at 1%. We were devastated and felt like our dream of having a family was slipping away. Our doctor recommended lifestyle changes and we started our first IVF/ICSI cycle. Seeing that single healthy sperm fertilize my egg on the screen was the most hopeful moment. Today, we have a beautiful baby girl, and we’re so grateful for the science that made it possible.”
Key Takeaways
The journey to understanding and addressing issues with morphology involves medical guidance, personal commitment, and often, advanced reproductive technologies. While a diagnosis can feel overwhelming, it is a manageable aspect of male fertility. Remember that a low percentage of normal sperm does not eliminate the possibility of conception, and numerous effective strategies exist to improve outcomes. Collaborating with a fertility specialist to explore all available options is the best way to navigate this challenge. Ultimately, improvements in morphology and successful conception are achievable goals for many couples.
- Definition: Sperm morphology is the analysis of the size and shape of sperm, a key factor in male fertility.
- Causes: Abnormal morphology can result from genetics, hormonal issues, lifestyle choices (smoking, diet), and environmental exposures.
- Diagnosis: It is diagnosed via a semen analysis, with Kruger’s strict criteria being a common evaluation method (≥4% normal is a reference point).
- Symptoms: There are no outward symptoms; difficulty conceiving is the primary sign.
- Treatment: Options range from lifestyle changes (diet, exercise) and supplements to medical procedures (varicocelectomy) and assisted reproductive technologies like IVF with ICSI.

Frequently Asked Questions (FAQs)
Can a man with 0% normal sperm morphology have a baby?
Yes. While challenging, conception is possible, often requiring assisted reproductive technologies like IVF with ICSI, where a single healthy-looking sperm is selected and injected directly into the egg.
How long does it take to improve morphology?
Sperm production takes about 74 days. Therefore, any lifestyle changes or treatments will require at least two to three months to show a potential effect on a new batch of sperm.
Does abnormal morphology cause birth defects?
Most research indicates that poor morphology is not directly linked to an increased risk of birth defects. The primary issue is the sperm’s ability to fertilize an egg, not the genetic quality of the embryo.
What is the best diet for improving sperm morphology?
A diet rich in antioxidants is beneficial. Focus on fruits, vegetables, whole grains, lean proteins, and healthy fats. Foods high in zinc, selenium, and folate are particularly helpful for sperm health.
Can you conceive with 2% sperm morphology?
Yes, conception is possible even with 2% sperm morphology, though it may be more challenging.
Can you improve sperm morphology?
Yes, lifestyle changes, medical interventions, and specific treatments can contribute to improving morphology.
What does 3% sperm morphology mean?
A 3% semen morphology indicates that only a small percentage of sperm have a normal shape, which may impact fertility.
Should I worry about sperm morphology?
While it can be concerning, low semen morphology should be discussed with a healthcare professional to assess its implications on fertility.
References
- World Health Organization. (2010). WHO laboratory manual for the examination and processing of human semen (5th ed.).
- Agarwal, A., Mulgund, A., Hamada, A., & Chyatte, M. R. (2015). A unique view on male infertility around the globe.
- Measurement and significance of sperm morphology – Menkveld R et al., Asian J Androl. 2010.
- Relationship between sperm morphology and sperm DNA dispersion – Jakubik-Uljasz J et al., Translational Andrology and Urology. 2020.