The uterus is a crucial organ in a woman’s reproductive system, and any abnormalities can significantly impact her ability to conceive and carry a pregnancy to term. One such condition is a bicornuate uterus, which affects approximately 1 in 200 women and can cause fertility issues.
A bicornuate uterus is a heart-shaped or two-horned uterus different from the typical pear-shaped one. Additionally, women with a bicornuate uterus may require specialized care during pregnancy.
If you or someone you know has a bicornuate uterus, it’s essential to understand the causes, symptoms, diagnosis, and treatment options to ensure the best chances of a healthy pregnancy.
Meaning of Bicornuate Uterus
A bicornuate uterus, also known as a heart-shaped uterus, is a type of congenital uterine malformation where a woman’s uterus is divided into two sections by a septum or wall of tissue.
This can cause issues during pregnancy, as the shape of the uterus may interfere with the baby’s growth and cause complications during delivery. The condition is most commonly diagnosed during prenatal ultrasound.
Also read – What is Bulky Uterus?
What are the Types of Bicornuate Uterus?
Your bicornuate uterus may be classified as complete or partial (incomplete) by your doctor. These words describe the depth to which your uterus descends from its uppermost point towards the cervix.
- Partial Bicornuate Uterus: It is one in which the two cavities are less separated from one another. The indentation that separates your uterus is less pronounced, but it still has a heart shape.
- Complete Bicornuate Uterus: A full bicornuate uterus is characterised by a significant indentation at the top of the uterus, which helps to distinguish the uterine cavity.
Is a Bicornuate Uterus Safe?
No, having a bicornuate uterus is not safe, but it is essential to note that while this condition can have profound implications, it is not life-threatening, and it is possible to have a successful pregnancy and delivery. However, women with a bicornuate uterus should be monitored more closely during pregnancy, and they may need to take certain precautions to ensure safe delivery.
How Does a Bicornuate Uterus Affect Fertility?
In most cases, a bicornuate uterus doesn’t affect fertility, but it can make it harder for you to carry a pregnancy to full term. This is because the unusual shape of the uterus may not have enough space for the baby to grow properly. It also increases the risk of:
- Early miscarriage
- Preterm labor (giving birth too early)
- Baby being in the wrong position (like breech) at birth
So, while a bicornuate uterus does not usually cause infertility, it can lead to pregnancy complications that need careful monitoring by a doctor.
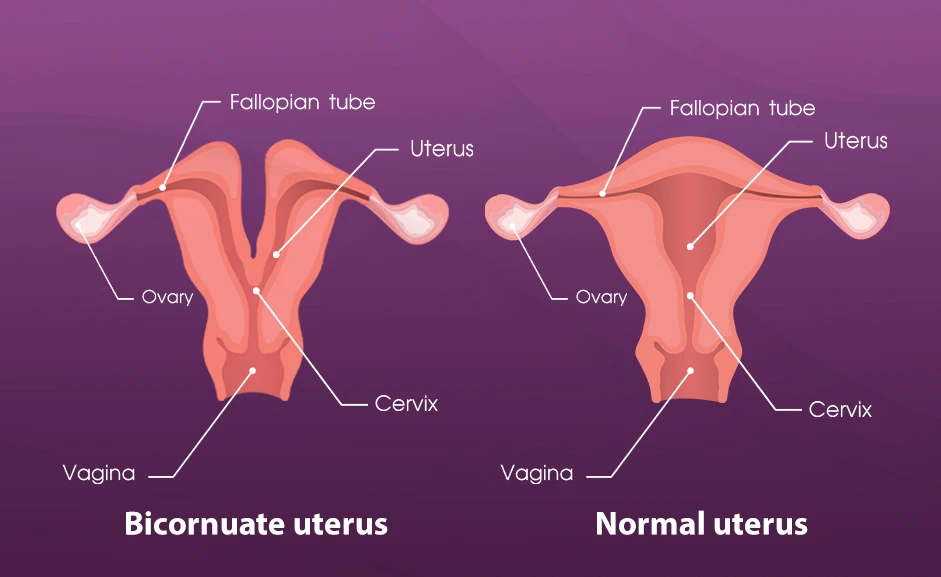
What is the Difference Between A Bicornuate Uterus and a Normal Uterus?
Although it is not easy to distinguish between the two if you haven’t gone for a diagnosis or faced multiple miscarriages but here is how it can be differentiated:
| Feature | Normal Uterus | Bicornuate Uterus |
| Shape | Pear-shaped with a single cavity | Heart-shaped with two cavities (horns) |
| Number of cavities | One central cavity | Two separate cavities, often unequal |
| Menstrual cycles | Regular and normal | Usually normal and unaffected |
| Fertility | No impact on conceiving | Usually no impact on conception |
| Pregnancy risks | Lower risk of miscarriage or preterm birth | Higher risk of miscarriage, preterm birth, or breech baby |
| Detection | Not detected on imaging (normal) | Detected on ultrasound, MRI, or HSG |
| Treatment needed? | No treatment required | Usually, no treatment unless recurrent pregnancy loss occurs |
| Prevalence | Most common (normal anatomy) | It is a rare condition affecting about 1–5% of women |
How to Recognise a Bicornuate Uterus?
Women with a bicornuate uterus are typically unaware of their unique uterine shape unless they have undergone an ultrasound or other diagnostic imaging test.
However, in some cases, you might experience the following:
- Painful menstruation
- Heavy bleeding (menorrhagia)
- Pelvic pain & discomfort
- Painful intercourse
- Vaginal bleeding
It is essential to understand that these symptoms do not solely signify the presence of a bicornuate uterus. It is always a good idea to consult with a fertility specialist in Delhi to diagnose the condition and choose a more effective treatment option.
What are the Causes of a Bicornuate Uterus?
A bicornuate uterus is a congenital abnormality that a woman is born with. This condition arises when a fetus’s uterus fails to develop normally in the womb due to the incomplete fusion of specialised ducts, resulting in a division of the upper part or horns of the uterus.
However, the exact cause of this abnormal development is unknown. Still, in some cases, it is believed to be due to genetic factors, hormonal imbalances, or exposure to environmental toxins during embryonic development.
Additionally, certain medical conditions, such as polycystic ovary syndrome (PCOS) and endometriosis, have been linked to an increased risk of bicornuate uterus.
Unfortunately, this condition is not preventable or reversible once it is present in an individual.
When Should I Visit a Doctor for a Bicornuate Uterus?
If you have pelvic pain during menstruation or intercourse, or if your vaginal bleeding is irregular, get in touch with a fertility expert or a gynaecologist. These indicate that the uterus is bicornuate.
Does a Bicornuate Uterus Affect Pregnancy?
Yes, a bicornuate uterus can affect pregnancy, but with proper diagnosis, doctor’s consultation and personalised treatment, you can still become pregnant.
The bicornuate uterus may impact pregnancy outcomes, although the extent of the impact may vary. The condition can lead to a higher risk of complications during pregnancy, such as:
- Miscarriage
- Preterm delivery
- Fetal malpresentation
- Cesarean delivery
- Low birth weight
- Vaginal bleeding
Additionally, there may be a greater likelihood of fetal growth restriction and placenta previa, where the placenta partially or fully covers the cervix. However, many women with a bicornuate uterus have successful pregnancies and deliver healthy babies.
Note: Women with this condition must receive prenatal care from a healthcare provider experienced in managing high-risk pregnancies. With close monitoring and appropriate management, most women with a bicornuate uterus can have a safe and healthy pregnancy.
How is a Bicornuate Uterus Diagnosed?
Most women aren’t aware of having a heart-shaped uterus until they undergo pregnancy or a checkup or repeated miscarriage. Here’s how your doctor will diagnose you if you have certain symptoms.
- Physical Examination and Ultrasound: Diagnosing begins with a physical exam and ultrasound, typically revealing the distinctive shape. During an ultrasound, the technician will look for the uterus’s distinct “heart-shaped” shape.
- MRI Scan: An MRI can also detect a bicornuate uterus and may be used if the ultrasound is inconclusive.
- Additional Tests: Certain tests, such as hysterosalpingography and hysteroscopy, can be used to evaluate the structure of the uterus and surrounding organs.
Although it can cause fertility issues, and it is often asymptomatic, and many women are unaware that they have the condition until they start trying to conceive.
It can worry expectant mothers, but it is essential to remember that it can be managed with proper care and monitoring throughout the pregnancy.
Can a Bicornuate Uterus be Treated?
Yes, a bicornuate uterus can be treated. While this condition is not life-threatening, it can cause significant discomfort and fertility issues. Fortunately, there are several treatment options available for women with a bicornuate uterus.
Hormone Therapy
One option is to use hormone therapy, which can help reduce the horns’ size and improve fertility.
Surgery
Surgical correction may be recommended for women with severe malformations that affect fertility or lead to recurrent miscarriages.
Assisted reproductive technology (ART)
Women with a bicornuate uterus may sometimes require assisted reproductive technologies, such as in vitro fertilisation (IVF), to conceive.
Cerclage
A cerclage is a procedure in which a stitch is placed around the cervix to help keep it closed during pregnancy. Women may require this procedure to prevent premature labour and miscarriage.
Progesterone therapy
Progesterone is a hormone that helps to support a healthy pregnancy. Women with a bicornuate uterus may require progesterone therapy to reduce the risk of preterm delivery.
Can I Still Become a Parent if I Have a Bicornuate Uterus?
Yes, even if you have a bicornuate uterus, you can still become a parent. Though you run a higher risk of pregnancy difficulties. The main cause of this is that your uterus cannot grow to accommodate your unborn child.
Your doctor will go over any safety measures you should take while pregnant, as well as the potential effects of having a heart-shaped uterus on your pregnancy and delivery.
A Word From Crysta IVF
Diagnosing a bicornuate uterus can understandably cause anxiety and uncertainty for women hoping to become pregnant. However, it’s essential to recognise that many people with this condition go on to have healthy pregnancies and deliver healthy babies.
With the proper medical care and support from qualified healthcare providers experienced in managing high-risk pregnancies, women with a bicornuate uterus can safely carry their pregnancies to term.
At Crysta IVF, we understand the challenges of infertility and high-risk pregnancies. We have helped many couples achieve their dream of parenthood and are committed to providing compassionate, individualised care to all our patients.
Frequently Asked Questions
Does a bicornuate uterus affect fertility?
No, usually most women with a bicornuate uterus can get pregnant naturally. But it can increase the risk of miscarriage or preterm birth because of the limited space in the uterus.
Can you carry a baby full term with a bicornuate uterus?
Yes, many women carry a baby to full term. However, there is a higher chance of early labour or needing a cesarean delivery if the baby is in an unusual position.
How is a bicornuate uterus diagnosed?
It is usually detected through imaging tests like an ultrasound, MRI, or hysterosalpingography (HSG). Sometimes it’s only discovered during pregnancy or after a miscarriage.
Does a bicornuate uterus cause pain or period problems?
Not usually. Most women with a bicornuate uterus have normal menstrual cycles and no symptoms unless they develop complications during pregnancy.
What are the risks of pregnancy with a bicornuate uterus?
Risks of pregnancy with a bicornuate uterus include:
- Miscarriage (especially in early or mid-pregnancy)
- Preterm delivery
- The baby is in a breech position
- Low birth weight
Can a bicornuate uterus be treated?
Yes, a bicornuate uterus can be treated, but if it’s not causing problems, no treatment is needed. In some cases of repeated pregnancy loss or severe symptoms, surgery (called metroplasty) can correct the shape.
Is a bicornuate uterus common?
It’s not very common; it affects about 1–5% of women, depending on the population studied.
Can you have a normal delivery with a bicornuate uterus?
Yes, but it depends. Some women can have a normal vaginal delivery, but many need a cesarean because the baby may be in an abnormal position.
What’s the difference between a bicornuate uterus and a septate uterus?
Both are uterine abnormalities, but in a bicornuate uterus, the outer shape is also abnormal (heart-shaped), while in a septate uterus, the outside is normal and a wall divides the inside.